
Foods for a Healthy Gut
Some foods are excellent for supporting our digestion and here are some of my favourites that I suggest to clients on a regular basis:
Cruciferous vegetables
These fab veg bring amazing health benefits on a number of different levels. Since we’re talking about foods that are helpful for your digestion, you should know that they contain compounds called glucosinolates, which are fermented by bacteria and used as fuel. They are prebiotic.
Examples include: Bok choy, broccoli, Brussels sprouts, cabbage, cauliflower, kale , rocket, spring greens, watercress.
Fermented foods
Fermented foods have a long tradition in some parts of the world, especially Asia, Africa, and Eastern Europe. Bacteria (and sometimes beneficial yeasts) might be involved in the process and the result is an increase of good bacteria in the foods. You’ve probably heard of live or ‘bio’ yoghurt.
Some of these other probiotic foods might sound peculiar and a little ‘advanced’ for most regular people. However, they are now commonly found on supermarket shelves and, while they might not be the kind of product you would usually go for, it is always worth experimenting. Kimchi, in particular, is often combined with chilli and other flavours and is far tastier than its name might suggest.
Examples include yoghurt, pickles (gherkins), sauerkraut, kimchi (fermented cabbage), tempeh (fermented soya beans), natto (fermented soya beans), miso soup (fermented soya beans), tamari soy sauce, buttermilk, some cheeses like cottage cheese, gouda, mozzarella and cheddar.
Fermented drinks
Like other fermented products, these were once only found in health food shops and were perhaps the prevail of people who ate a very clean and unprocessed diet.
These were a secret waiting for the masses to discover. Often flavoured with fruits, they really are delicious and do not taste 'worthy'. You'll find them in the chilled drinks section in most supermarkets.
Kombucha (fermented tea - sweet and fizzy but without sugar) and kefir (fermented dairy drink very much like a yoghurt drink) are examples.
The only way you’ll know if it’s for you is to try!
Fibre
Fibre is one of the best things to eat to support healthy digestion. Fibre is described as being either insoluble or soluble.
This is part of the plant wall in fruit and veg. It’s indigestible so it passes right through your system, sweeping up toxins and other waste products as it goes, and keeping you regular. The undigested fibre is also fermented by gut bacteria, producing the beneficial short chain fatty acids mentioned earlier.
YOU CAN FIND INSOLUBLE FIBRE IN:
Fruit and veg, beans and lentils, oats and wholegrain foods like brown rice and wheat.
This can be partially digested and is well-celebrated for its ability to reduce cholesterol in the blood and normalise blood sugar levels.
YOU CAN FIND SOLUBLE FIBRE IN:
Oats, veg, fruit (especially apples, pears, berries, and citrus fruits), beans and lentils.
Anti-Microbial Foods
Some foods exert a natural antibiotic or anti-fungal effect and can be useful for keeping nasties like pathogenic bacteria or unwelcome yeasts at bay.
These include caprylic acid found in coconut. Coconut oil is also a very good oil to use in cooking, especially at high temperatures.
Garlic contains the active ingredient allicin, which has historically proven itself to be an effective killer of both bacteria and viruses, making it a great immune-boosting ingredient. Use it raw wherever possible.
Olive oil – the oleic acid has anti-bacterial properties. Use it generously to dress salads and veg.
And we can’t have a list of the foods to add in, without looking at what we need to avoid for a happy tummy:
Sugar and refined carbohydrates
In same way there are things your digestive system loves, there are things it will not love you for. Sugar. That’s the number one thing to avoid, plus anything that contains added sugar.
Other things your tummy is not fond of include highly refined products like white rice, pasta, pastry and snacks like crisps and biscuits.
If you would like to take a look at your gut health – whether you have symptoms or would just like to be optimally well – why not book in a free call? You can book via the link.

Understanding Endometriosis vs. PCOS
It is Endometriosis Awareness Month this month. Endometriosis affects about 1.5 million women in the UK, but it remains one of the most under-diagnosed conditions.
While we are PCOS specialists here at PCOS Clinics, we often see women with endometriosis as well as PCOS in clinic. So, what’s the difference?
Endometriosis and polycystic ovary syndrome (PCOS) are two common conditions that affect women. While both conditions can cause menstrual irregularities and fertility challenges, they differ in their underlying hormonal imbalances, symptoms, and treatment approaches. Understanding these differences is key to seeking the right diagnosis and treatment.
Endometriosis vs. PCOS: How They Differ
Both conditions can lead to heavy menstrual bleeding and issues with fertility, but they have distinct causes and symptoms:
Symptoms of Endometriosis vs. PCOS
|
Symptom |
Endometriosis |
PCOS |
|
Heavy bleeding |
Yes |
Yes |
|
Irregular periods |
Rare |
Yes |
|
Painful periods |
Yes |
Sometimes |
|
Pelvic pain |
Before periods |
Any time |
|
Pain during or after sex |
Yes |
No |
|
Painful urination or bowel movements |
Yes |
No |
|
Excess body hair |
No |
Yes |
|
Hair loss on head |
No |
Yes |
|
Acne and oily skin |
No |
Yes |
|
Fatigue and low energy |
Yes |
Yes |
|
Weight gain |
No |
Yes |
|
Bleeding without ovulation |
No |
Yes |
Prevalence of Endometriosis and PCOS
What Causes Endometriosis and PCOS?
Endometriosis Causes
While the exact causes are not yet known, the following hypotheses have been put forward:
PCOS Causes
Who is at Risk?
Risk Factors for Endometriosis
Risk Factors for PCOS
Can You Have Both Conditions?
Yes. Studies suggest a strong link between PCOS and endometriosis, particularly in individuals experiencing pelvic pain or infertility.
High androgen and insulin levels in PCOS may contribute to anovulatory periods (periods where we don’t ovulate), which may lead to higher levels of oestrogen, potentially exacerbating endometriosis.
Conventional Treatment Options for Endometriosis and PCOS
Endometriosis Treatment
PCOS Treatment
When to See a Doctor
Seek medical advice if you experience:
Early diagnosis is crucial for symptom management. A gynaecologist or endocrinologist can provide a tailored treatment plan.
Final Thoughts
Endometriosis and PCOS are distinct but often misunderstood conditions that can significantly impact overall health.
While endometriosis results from excessive oestrogen and misplaced uterine tissue growth, PCOS stems from an overproduction of androgens, leading to metabolic and reproductive complications. If you suspect you have either condition, early medical intervention can help manage symptoms and improve quality of life. And don’t forget the power of diet and lifestyle changes – if you’d like to know more, get in touch.

Your hormone balancing action plan
If you’re looking to balance your hormones, here are my five top tips:
Prioritise sleep
There are some actions you can take to make a good sleep much more likely. These include things like avoiding drinks containing caffeine after lunch, going to bed at the same time every day, keeping the temperature in your bedroom comfortable, keeping the bedroom completely dark so you’re not disturbed by light and making an effort to relax for at least 5 minutes before going to bed - a warm bath, massage, meditation and so on.
The biggest tip I can give you is to really ensure that you prioritise your sleep. Make a real effort to focus on all the things you can do to improve your sleep hygiene rather than ‘kind of’ doing it.
Move your body
Exercise can have a noticeable effect on hormones and mood. You might have heard how exercise releases endorphins and the feel-good hormones dopamine and serotonin.
Instead of moving in such a way that you place excessive stress on the body, consider how your body likes to move. Focus on things like brisk walks, yoga or pilates, and weight training ahead of more punishing regimes involving spin classes and long runs.
Improve your digestive health
There might seem quite a geographical distance between your digestive system and your brain but the two are actually very closely connected. In fact, the digestive system is often referred to as the ‘second brain’.
If you have any problems with your digestive system, it will be worth working on these with a nutrition professional. Your nutritionist will be able to advise if any functional testing might be appropriate to look for food reactions (allergies or intolerances) or a broader test to see whether you might have bacterial imbalance or infection.
For the purposes of this blog, it might be helpful to ensure you regularly eat probiotic foods like natural yoghurt, kefir and kombucha (all are now widely available even in supermarkets) or even take a probiotic supplement.
Reduce stress
Taking action to reduce stress in your life is essential but many people are concerned the specific things they might do are too much of a luxury in their already-busy lives.
Bottom line: you can’t simply keep going the way things are.
Taking some time to empty the ‘stress bucket’ is critical for your wellbeing. Yoga and mindfulness/meditation are proven ways to reduce stress but consider taking time out just to do the things you love to do quietly, mindfully and on your own: sitting in the garden with a cuppa, reading, colouring, knitting, or trying out a new hobby.
Balance your blood sugar
Blood sugar levels have a profound effect on our hormones largely due to the effect they have on insulin, which has a knock-on effect to our sex hormones. Balancing blood sugar could be an entire blog in itself, so do check back on previous blogs I have written.
But, in essence, try to stick to three good meals per day, and avoid snacks unless absolutely necessary. Make sure to have good quality protein with every meal and/or snack, and make sure that half your plate is covered with veggies (the green and brightly-coloured kind – not potatoes!)
And don’t forget, I’m always here if you’d like to discuss hormone testing or look further into why your hormones might be acting up right now. Just book in a call here.

Healthy, happy hormones
When you think about mental health, you’re probably thinking about your brain and how that works. The picture is often much more complex. Hormones play a big part because these chemical messengers are the background to everything that happens in your body. How you feel, therefore, is not just psychological, it’s biological.
Did you know, there are a huge number of symptoms that are common to both depression and hormonal imbalance? These include low energy, dizziness, low mood, apathy, anxiety, irritability, anger, lack of enthusiasm, despair, headaches, poor concentration, feelings of hopelessness, lack of confidence, low libido, fuzzy brain, memory loss, and insomnia (although there are others).
Rebalancing your hormones naturally is not something that happens overnight, but it can be greatly improved with the help of nutritional and lifestyle change. This blog will allow you to pinpoint where you might need help or support.
Mood and your cycle
Two of the main hormones that affect your feelings of mental wellbeing and clarity are oestrogen and progesterone, and these change throughout your menstrual cycle. It’s an over-simplification – but perhaps a helpful one – to think about oestrogen largely bringing positive effects to your mood and progesterone contributing more negative effects. With such a pronounced hormonal connection on mental health, it’s small wonder that women are twice as likely to suffer from depression than men.
According to the National Institute of Mental Health, 64% of women who suffer from depression say their symptoms get worse during the pre-menstrual period. Hormones are also likely to contribute to antenatal or postnatal depression, which affect around 10-15% of new mothers. And anxiety and depression are also starting to be recognised as symptoms of the peri- menopause on top of hot flushes and night sweats.
How it works
At certain times in your cycle (in the run-up to ovulation), there will be lots of oestrogen in your system and women tend to feel brighter and better in their mood. You might even notice at this time you feel better at talking and articulating yourself. In the second half of your cycle, oestrogen dips and progesterone comes into play. For some women, this can lead to lowered mood or depression.
PMS or PMDD
You might already experience this as Pre-menstrual Syndrome (PMS), a very common condition linked to the changing levels of these hormones, that might include feelings of bloating, breast tenderness or headaches, or manageable emotional symptoms like irritability.
For a small number of women (about 2-8%), the effect of these hormones on their mental wellbeing is pronounced. This is called Pre-menstrual Dysphoric Disorder (PMDD); an extreme form of PMS and one that, if you think might apply to you, you will want to ask your doctor about.
Why does this happen?
One of the first things to know is that the production of dopamine and serotonin (the two main brain chemicals associated with the development of depression and psychosis) is heavily linked to levels of oestrogen.
Research seems to suggest that there isn’t a noticeable difference in levels of oestrogen between those who are affected by mental health symptoms around their period or during the menopause – it seems some women are just especially sensitive to hormonal change, or perhaps also that lifestyle problems like stress may also play a big part.
Other hormones
Testosterone:
You might think of testosterone as the male hormone and, while men do produce much higher levels, every woman needs testosterone, too. Testosterone can increase sexual desire and libido, make bones and muscles strong, and have you feeling assertive and confident. The downside can be anger and aggression. For us women with PCOS, we can suffer from an excess of testosterone and other androgens, which comes with its own set of issues.
Thyroid:
Altered levels of thyroid hormones impact on mental wellbeing. If you just don’t feel like yourself, feel lethargic and low, it could be that your levels of active thyroid hormone are low. This can often run hand in hand with PCOS and it’s important for you to have it checked out.
Cortisol:
Cortisol is one of the main stress hormones and, when stress levels are high, literally any of the mood-related symptoms I have mentioned in any of the above might be present.
Oxytocin:
Oxytocin directly opposes cortisol. It’s the love hormone and, if you have children, you might recognise it as the hormone that floods women after childbirth to encourage bonding. It has a direct effect on appetite, insulin resistance, weight loss – and your mood.
Impact of hormones on your blood sugar levels
Low oestrogen levels have a role to play in insulin sensitivity (that means how sensitive – or not – the cells in your body are to the fat storage hormone insulin). In fact, a lack of sensitivity to insulin (or even being resistant to the effects of insulin) is lurking behind many of the common hormonal symptoms in PCOS, like fatigue and weight gain as well as symptoms of low mood like brain fog, anxiety and depression.
“Hormones and mental health” is a complex picture in which your physiological health and mental wellbeing are inextricably intertwined. It’s best to work with a nutrition practitioner to unravel this for you. They will be able to piece together a hormone balancing food and lifestyle plan to suit your circumstances. Check out my Hormone Balancing Action Plan or why not book in a call here?
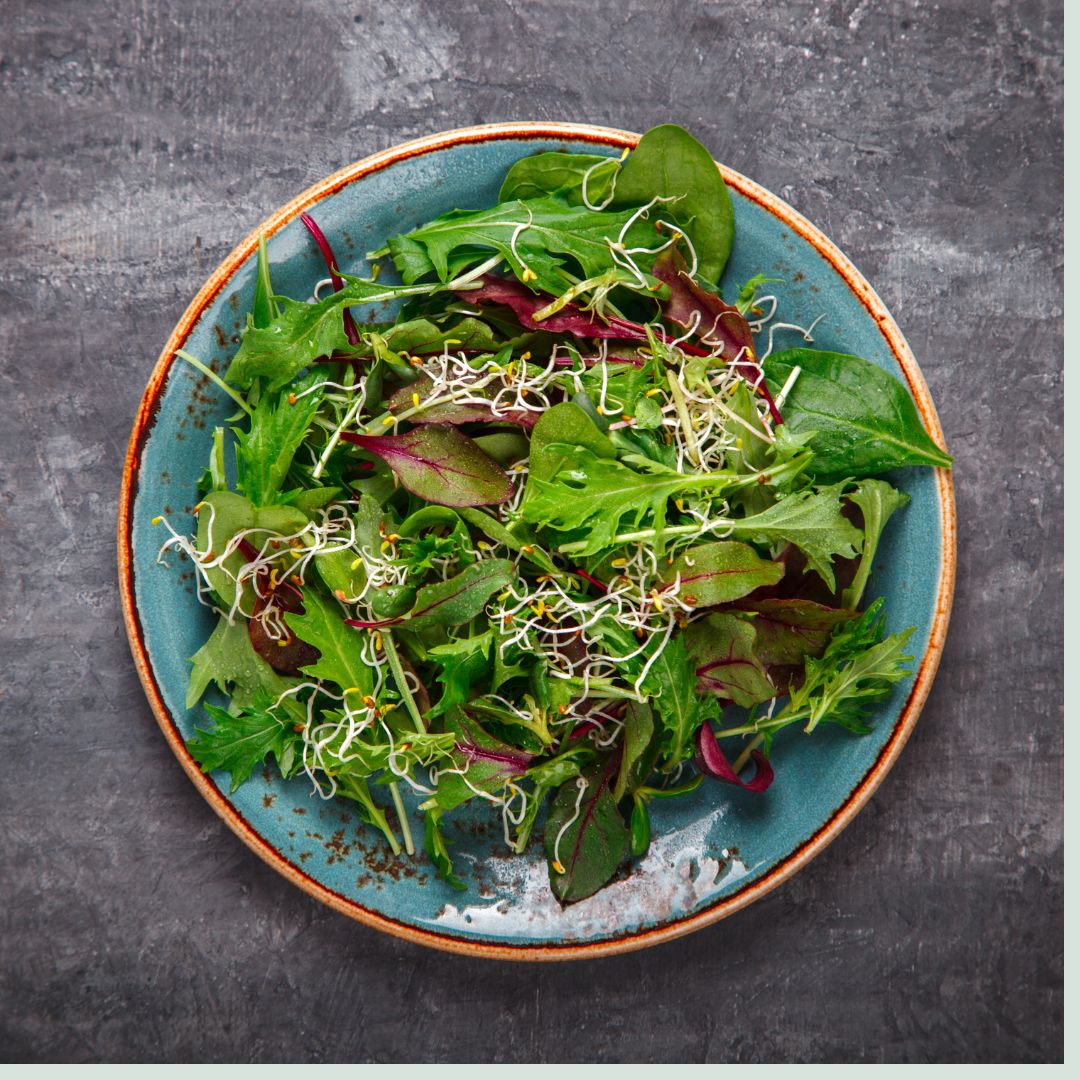
Nutrition hack: Eat a Salad Before Your Main Meal
Here is a fab, straightforward and effective blood sugar balancing hack that incorporates the benefits of fibre, greens, and a secret ingredient – apple cider vinegar.
Let's explore the science behind this hack and discover how it can contribute to hormonal balance, particularly for those of us with PCOS.
The Science of High-Fibre Foods
Scientists have long acknowledged the impact of high-fibre foods on gastric emptying, the process by which food leaves the stomach. High-fibre foods, like salads, slow down this process, influencing the rate at which glucose and other nutrients are delivered to the small intestine for absorption into the bloodstream. By incorporating a light, green salad at the start of your meal, you can effectively slow down the absorption of glucose, preventing sudden spikes in blood sugar levels.
Avoiding Blood Sugar Spikes and Insulin Surges
The key benefit of commencing your meal with a fibre-rich salad lies in avoiding blood sugar spikes. When glucose enters the bloodstream gradually, it diminishes the need for a rapid insulin response. This, in turn, aids in balancing hormones and may be particularly beneficial for individuals dealing with conditions like Polycystic Ovary Syndrome (PCOS).
Apple Cider Vinegar: A Secret Weapon
To enhance the blood sugar balancing effect, consider dressing your salad with a homemade vinaigrette that includes apple cider vinegar, preferably one that contains the "mother." A 2015 crossover, randomized study suggested that apple cider vinegar may play a role in improving the body's absorption of blood sugar and increasing insulin sensitivity in skeletal muscle. This double whammy approach – combining fibre-rich greens with an apple cider vinegar dressing – can be a powerful addition to your blood sugar balancing arsenal.
Crafting a Blood Sugar-Friendly Salad
Now that we've explored the science behind this blood sugar balancing hack, let's create a delicious and nutritious salad that incorporates these principles:
Ingredients:
Fresh mixed greens (spinach, kale, rocket)
Colourful vegetables (tomatoes, cucumbers, peppers)
Homemade vinaigrette dressing (olive oil, apple cider vinegar, Dijon mustard, herbs)
Optional: nuts or seeds for added crunch and nutrient boost
Instructions:
- Start your meal with a generous serving of fresh mixed greens.
- Add an assortment of colourful vegetables to boost the nutritional content.
- Prepare a homemade vinaigrette dressing using olive oil, apple cider vinegar, Dijon mustard, and your favourite herbs.
- Toss the salad gently, ensuring an even coating of the dressing.
- Optionally, sprinkle nuts or seeds on top for added texture and nutrient richness.
Incorporating a light green salad with an apple cider vinegar dressing into your meals can be a simple yet impactful strategy for maintaining balanced blood sugar levels.
By understanding the science behind this hack, you empower yourself to make informed dietary choices that support overall health and well-being. Give it a try, and let us know about your experience with this blood sugar balancing approach!

Lean PCOS and Its Unique Challenges
While PCOS is often associated with weight gain, lean PCOS presents its own set of challenges, marked by hormonal imbalances and symptoms that may not be immediately obvious. PCOS typically conjures an image of weight gain and hormonal imbalances, but lean PCOS challenges this stereotype. In lean PCOS, individuals may have a relatively normal body mass index (BMI) but still experience the hallmark symptoms of the condition. It's a lesser-understood variation that requires special attention and awareness.
Signs of Lean PCOS
The subtlety of lean PCOS symptoms emphasizes the importance of recognising and addressing this unique presentation of the condition. Here are some symptoms that lean PCOS may be a factor in your experience:
Exploring the intricacies of lean PCOS involves understanding how hormonal imbalances and metabolic factors contribute to its unique challenges:
Managing Lean PCOS
Recognizing lean PCOS helps those of us with it to adopt a specialised approach to management, focussing on hormonal balance and overall wellbeing.
If you’d like to find out more about how you can manage lean PCOS through diet and lifestyle, why not book a free call with our team – just click here to book.